Getting closer to answers at the Cleveland Clinic through perseverance, communication, and patience
I mentioned in my last Cleveland Clinic update that one of my November MRIs had revealed a tumor in my spine. However, until I had a consult with one of my neurologists, I was not clear on the significance of this tumor in relation to my symptoms. I had a virtual consultation with Dr. Shuaib on December 22nd. The tumor is located within my T10 vertebrae and is labeled an Intraosseous Hemangioma. Intraosseous Hemangiomas are benign vascular tumors that account for less than 1% of all bone tumors. An injury to, or tumor in, the T10 vertebrae would affect one’s lower abdomen, buttocks, legs, and feet. Check, check, check, and check.
However, my tumor is completely encased in bone within the T10 vertebrae. It is not impinging on my spinal cord, and therefore, is not responsible for the symptoms I’ve been dealing with for over two years. I’m not entirely sure how to feel about this. I mean…it’s not like I was hoping for a spinal tumor. Who would?!? However, if it could mean an answer to everything…along with a solution…who wouldn’t?!?
what now
So…what now? Where do we go from here?
Dr. Shuaib has two paths he would like to explore and Dr. John, another of my neurologists, has a third path. The dilemma they are working out is whether to completely explore the two directions of Dr. Shuaib before beginning to look into the path Dr. John thinks it could be. Or…simultaneously explore all three paths. As is often the case, there are advantages and disadvantages to both avenues.
Regardless of which avenue is eventually agreed upon, the biggest takeaway here is that they are continuing to explore. And for that…I am beyond grateful.
looking ahead to march
My thoughts and emotions are all over the place with what I’ll be sharing…so bear with me, please…I think you’ll understand why as you read further.
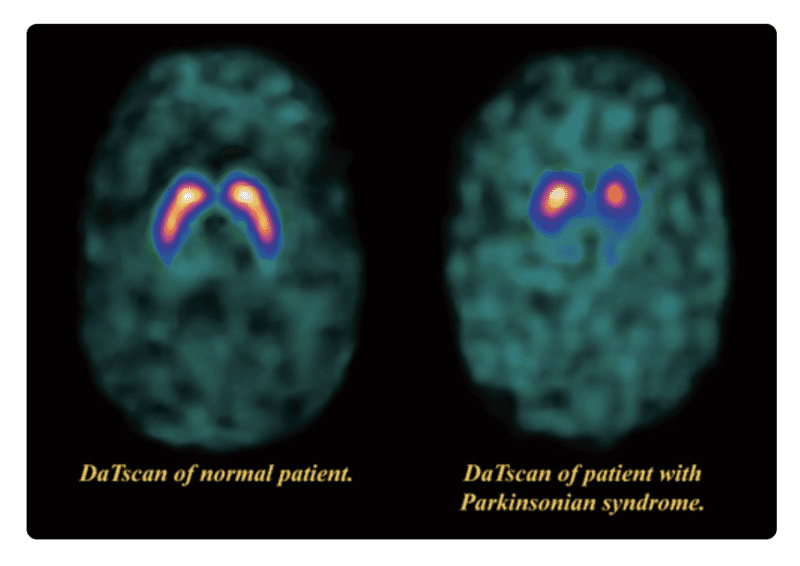
I will head back to the Cleveland Clinic in mid-March for 3 days of additional consultations and imaging. We will arrive in Cleveland in the evening on Tuesday, March 14th to an extremely full schedule for Wednesday. Dr. Shuaib has ordered a DaTScan, an imaging tool used to confirm the diagnosis of Parkinson’s Disease. I will go into Nuclear Medicine around 9:00 am for an injection of the tracer and return 4 hours later for the actual scan. And, yep…you read that right. It is “an imaging tool used to confirm the diagnosis of Parkinson’s disease”. But…I was diagnosed by a neurologist over 5 years ago. I’ve been taking Parkinson’s medications for over 5 years. I’ve dedicated the last 3 1/2 years to Parkinson’s Disease awareness and advocacy. Confirmed…right?!?
And yet, now…a Movement Disorder Specialist at the Cleveland Clinic wants to do a scan to confirm whether I actually do have Parkinson’s Disease. He does feel that I likely do have PD, as a couple of my symptoms are trademark Parkinson’s symptoms. But, he also strongly feels that it is secondary to a broader, more complex neurological disease…Functional Neurological Disorder, FND…that is causing most of the complications.
what is functional neurologic disorder
Functional Neurologic Disorder features neurological symptoms that can’t be explained by a known neurological disease or other medical condition. However, the symptoms are real and cause significant distress or problems functioning.
Signs and symptoms vary, depending on the type of Functional Neurologic Disorder, and may include specific patterns. Typically, this disorder affects your movement and/or your senses, such as the ability to walk, swallow, see and hear. Symptoms can vary in severity and may come and go or be persistent. However, you can’t intentionally produce or control your symptoms.
The exact cause of Functional Neurologic Disorder is unknown. Theories regarding what happens in the brain to result in symptoms are complex and involve multiple mechanisms that may differ. Basically, parts of the brain that control the functioning of your muscles and senses may be involved, even though no disease or abnormality exists. Symptoms of Functional Neurologic Disorder may appear suddenly after a stressful event, or with emotional or physical trauma. Other triggers may include changes or disruptions in how the brain functions at the structural, cellular, or metabolic level. But the trigger for symptoms can’t always be identified.
back to “looking ahead to march”

This definition of FND explains why so many of my exams, images, and lab draws are coming back inconclusive or empty. And also explains why my March visit to the Cleveland Clinic is so full. Functional Neurologic Disorder, according to Dr. Shuaib, requires a team approach across several specialties. Following the injection for my DaTScan, I will meet with the Physical Therapy (and possibly Occupational Therapy) team. They will assess what I currently can and cannot physically do, formulate a treatment plan, and make a recommendation to therapists closer to home that can help execute their plan.
I will be matched with a small group of 5 or 6 other patients of Dr. Shuaib who either have a diagnosis of FND or are being assessed for FND. We will meet once a month virtually with Dr. Shuaib and/or a CC PsyD as an open forum, Q & A style support group.
I will head back to Nuclear Medicine for about 60-90 minutes for the actual DaTScan.
Eventually heading to my final, and in my opinion, most comprehensive appointment on Wednesday.
the psychology of it
I will meet with Dr. Hasnie, a Psychologist within the Neurological Restoration Center at Cleveland Clinic, and also a member of my new FND team.
When I met with Dr. Shuaib just before Christmas and he shared his assessment and thoughts with me, he stated that a diagnosis of Functional Neurologic Disorder is multi-dimensional. It is good news in that it is (finally) a much sought-after diagnosis and one with treatment possibilities and potentially, over time, a resolution. It is disappointing news in that it is a terribly challenging and heavy diagnosis with an equally challenging and extremely rigorous treatment plan.
A big piece of this treatment plan will be Dr. Hasnie…for many reasons.
First, this is a difficult diagnosis to receive and Dr. Shuaib believes that the support and guidance of a Psychologist are crucial to successful treatment. Second, he has learned, as well, that by the time a patient receives an FND diagnosis, they have often spent the last several weeks, months, or even years, feeling unseen, unheard, and ignored…at times even being accused of fabricating their symptoms. This is extremely damaging and must also be addressed within the treatment plan. It actually needs to be addressed across healthcare in general…but that is an enormous issue all on its own. And, third…Dr. Shuaib is adding the support of Psychology because simply put…I’m not okay.
not okay
Those of you that know much of my backstory know that I’ve struggled with depression in the past. That struggle became prominent again 5 years ago, following my Parkinson’s diagnosis. However, with some hard work and the help of a great therapist…the struggle was overcome. Until COVID. It has been 2 years and 2 months since I tested positive for COVID. And nothing, including my mental health, has been the same since.
From the moment I decided to share my story and my journey with (or maybe without) Parkinson’s, I promised myself and anyone reading that I would always be as real and raw and authentic as possible. Not for attention or sympathy…but for awareness and advocacy. For the hope and possibility that something I say or something I write might be the exact something that someone, someone possibly lost and stumbling through their own journey, is searching for. And right now…my real, raw, authentic self is not okay. I have participated in 3 separate mental health assessments for my care team at Cleveland Clinic. And, although I mostly seem (or so I thought) to “hide it well”…I have raised red flags with the team at each assessment.
I am severely depressed. I’m buried in grief. And I am carrying insane guilt for both of these feelings and more. I can only do a pitifully small fraction of the things I used to be able to do and even fewer of the things my family needs from me. I have lost friends. The sadness and guilt within those realities are tremendous. Again, I don’t share any of this in a quest for attention or sympathy…but rather, for awareness and advocacy. I will be okay…not right now…but someday. With hard work and help…I will, once again, overcome the struggle.
back to “what now”
Remember waaaay back up there 👆 in “what now” I mentioned Dr. John and that third path he would like to explore…? COVID. COVID is the path he’d like to explore. Could all of this be related to COVID and the ugly after-effects of Long-COVID? Even the diagnosis of Functional Neurologic Disorder, in which the cause is often unknown…? The cause may not be known, but symptoms of FND may appear suddenly after a stressful event, or with emotional or physical trauma. Other triggers may include changes or disruptions in how the brain functions at the structural, cellular, or metabolic level. Could COVID be that “physical trauma” or the origin of the “disruption of brain function“?
They don’t know because the long-term implications of COVID are too new…but they’re weighing the advantages and disadvantages, and the timing, of a referral to the Cleveland Clinic’s reCOVer Clinic. If they deem it advantageous at this time, they will try to coordinate that referral for the Thursday that I will already be in Cleveland. And then on Friday, I’m scheduled to wrap up my multi-day appointment(s) in a consultation with Dr. Shuaib to go over everything from Wednesday and Thursday…including the DaTScan…to confirm, or not, my diagnosis of Parkinson’s Disease.
all over the place
I warned you that my thoughts and emotions were all over the place as I began writing this. I only hope that you were indeed able to bear with me and that you do understand why.
This. Is. A. Lot. Hearing it was a lot. Writing it was a lot. Hitting “publish” will be a lot.
And right now…I’m also needing a lot. A lot of positive thoughts. A lot of prayers.
In addition to sorting out and absorbing all of this news and coordinating all of these consultations, I learned…just before Christmas…that while my primary medical insurance is covering the portion of the bills that they usually do, my secondary medical insurance will not be picking up the portion that they usually do. Because? My secondary insurance is issued for Michigan and I am receiving treatment in Ohio. And, I learned…just after Christmas…that my application for the financial assistance program sponsored internally by the Cleveland Clinic was denied. Because? I live in Michigan and the Cleveland Clinic is in…well…Cleveland, Ohio.
The trips to Cleveland Clinic…between fuel, food, & lodging and co-pays & deductibles…are not inexpensive.
And yet, I’m trying to hold onto the faith that somehow…things will work out. I will do all I can to find a way to continue making my way to Cleveland. I am too close to answers…too close to maybe getting my life back…to give up now.
Your love and your prayers are felt and now, especially… I selfishly covet them.
Thank you…from the bottom of my heart…to each and every one of you that continues to take a moment to check in on me. Your messages and your notes help bring light to my darker days. Your strength and your faith sustain me when fear weakens my own.
Despite all challenges and fears…blessings always abound.



Wow. You surely are my hero. Please know I think of you often and will keep you in my prayers. Thanks for sharing your journey.
I will continue to keep you in my prayers Nikki! Please take care as bedt you can! Hugs, Sue G.
I can certainly see why all this is overwhelming. So much to hear, absorb, process. And, yet, you and your family persevere, forming a plan with the medical community and move forward. I have no idea how draining this all is. You are all in my prayers.